Indentation Mechanics of Soft Materials
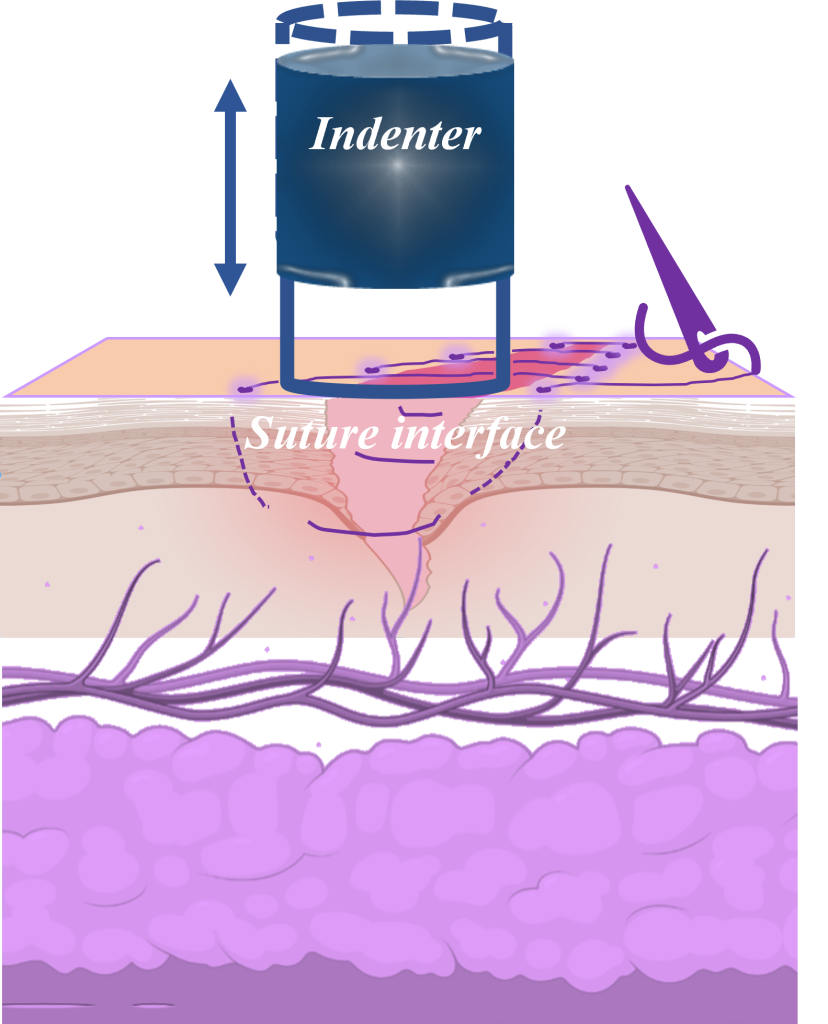
Our microindentation methodology, augmented by integration with high-resolution external imaging systems, permits the precise delineation of the interfacial contact profile between soft materials and the indenting device. This technique is particularly adept at uncovering time-dependent force responses of soft matter, such as adhesion and viscoelastic properties, without introducing observational bias. We have applied this technique to assess a variety of biological and synthetic substrates including engineered cardiac tissue microbundles, interfaces of sutured tissues, porcine myocardial tissue, and polydimethylsiloxane (PDMS) micropillars. Taking the sutured tissue interface as a representative study, we explore the use of nanoindentation to dissect the quasi-static and dynamic responses to stress at the junction of wounded and sutured tissues.
Through in vitro experiments and wound healing progression analysis, we gain insights into the mechanical integrity, modulus, and stability of tissue interfaces repaired using an artificial abdominal wall model. We observe that sutured tissues employing simple interrupted suturing (SIS) techniques exhibit a modulus that is approximately 35–40% greater than those closed with simple continuous suturing (SCS). Furthermore, sutured tissues with higher suture density, exemplified by a suture spacing of 2.5 mm, show a modulus that is roughly twice as high as that of tissues sutured at a lower density with a spacing of 5 mm. Additionally, the elastic modulus of sutured tissues, when immersed in deionized water, reaches about 70–95% of the modulus measured under dry conditions. Dynamic stress analysis reveals that suturing technique and suture density significantly influence the stability of stress at the wound interface under the influence of long-term bodily movements. The critical factors impacting wound healing efficacy, such as the quasi-static and dynamic moduli at the sutured junction, are closely linked with clinical outcomes, including patient discomfort, incidence of wound complications, healing rates, and blood circulation at the wound site.
The methodology and findings presented in our study offer a novel approach to addressing the dynamics of wound healing, contributing to patient welfare. They provide a foundational framework for re-evaluating existing paradigms in suturing techniques, potentially influencing the resolution of longstanding debates within the clinical community regarding optimal suturing practices.
